Introduction
The incidence of lymphoproliferative disorders (including plasma cell disorders) (LPD) and diabetes mellitus (DM) increase with age. The metabolic link between DM and multiple myeloma (MM) or LPD has been researched in other epidemiologic studies with a small number of cases suggesting an increased risk (Dankner et al Am J Epi 2016, Castillo et al Blood 2012). However, this link has not yet been studied in patients with related disorders such as monoclonal gammopathy of unknown significance (MGUS), AL amyloidosis (AL), or Waldenstrom macroglobulinemia (WM). This is the first study to evaluate the risk of DM on LPD in a large Swedish population-based case-control study.
Methods
We conducted a large population-based matched case-control study to evaluate the impact of a preceding diagnosis of DM on the development of a LPD. We included all cases of MM, WM, AL and other LPs (OLP) in the nationwide Swedish Cancer Registry and cases of AL and chronic lymphocytic leukemia (CLL) in the Swedish patient registry from 1987-2013. MGUS was acquired from a network of oncology and hematology clinics in Sweden. OLPs included the diagnoses of Hodgkin lymphoma, non-Hodgkin lymphoma, CLL, T cell lymphoma and other lymphocytic leukemias. For each case, up to four controls matched by age, gender, and county of residence from the general population were included. Cases with no controls were excluded. Diagnoses of DM were acquired from the Swedish patient registry where they were coded using ICD 9 and 10 codes. Conditional logistic regression was then performed controlling for the matching variables estimating the odds ratio (OR) of each LPD for a diagnosis of DM before the diagnosis of the LPD. OR of each LPD for the diagnosis of DM greater than one year and less than one year prior to the diagnosis of LPD was also calculated.
For MGUS cases, we also assessed the risk of progression to LPD. To avoid immortal time bias we include DM as a time dependent covariate in a Cox-model adjusting for age, sex, and year of MGUS diagnosis. All analyses were performed in R using the survival, and survminer packages.
Results
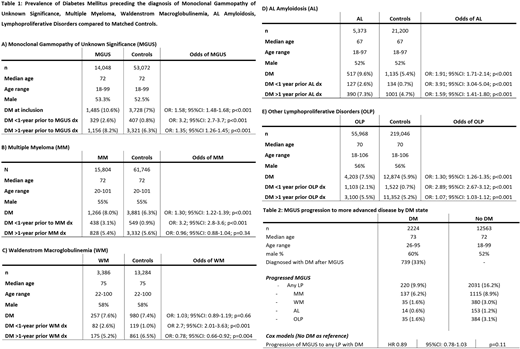
Patients with a diagnosis of MGUS (OR: 1.58; p<0.001), MM (OR: 1.30; p<0.001), AL (OR: 1.91; p<0.001) and OLP (OR: 1.30; p<0.001) are significantly more likely to have a preceding diagnosis of DM compared to matched controls whereas patients with WM are not (OR: 1.03; p=0.66). These results remained significant for MGUS (OR: 1.35; p<0.001), AL (OR: 1.59; p<0.001) and OLP (OR: 1.07; p=0.001) when only cases of DM > 1 year prior to the diagnosis were included (Table 1). However, patients with (vs. without) a diagnosis of DM are not more likely to progress from MGUS to MM, WM, AL or OLP (HR 0.89; p=0.11) (Table 2).
Discussion
The strength of our study lies in its large sample size and the availability of 4 matched controls for each case. The diagnosis of DM is associated with an increased risk of MGUS, MM, AL and OLP. This risk is greatest for DM diagnosis in the year prior to LPD diagnosis. This may be due to DM induced hyperglycemia leading to epigenetic changes that increase the odds of developing/accelerating early stage cancer given that they may have prediabetes/undiagnosed DM for many years prior (Huang et al Diabetologia 2014). It is also plausible that patients with DM for >1 year have been on metformin which has been shown to have a protective effect and are less likely to progress suggesting the role of hyperglycemia in its progression (Chang et al Lancet Haematol 2015). Alternatively, patients are likely to have DM diagnosed in the year prior due to similar symptoms of fatigue or weight loss, or a detection bias due to increased physician visits and laboratory testing. This lack of increased progression from MGUS in DM may be explained by the small numbers of patients that progressed in this dataset or the inability to control for factors such as DM treatment. Some other limitations include the lack of granular information related to DM, body mass index as well as prognostic information for the LPD.
Conclusions
Although, smaller prior studies have suggested a link between DM and cancer including MM and LPD, this is the largest study in patients with LPD. This is also the first epidemiologic study establishing a link between DM and MGUS as well as AL. Research into further understanding this association would enable us to provide patients with better treatment options in the future.
Shah:Physicians Education Resource: Honoraria; Celgene/BMS: Research Funding. Hultcrantz:Intellisphere LLC: Consultancy; Amgen: Research Funding; Daiichi Sankyo: Research Funding; GSK: Research Funding. Hassoun:Takeda: Research Funding; Celgene: Research Funding; Novartis: Consultancy. Korde:Astra Zeneca: Other: Advisory Board; Amgen: Research Funding. Lesokhin:BMS: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria; GenMab: Consultancy, Honoraria; Serametrix Inc.: Patents & Royalties; Janssen: Research Funding; Genentech: Research Funding; Juno: Consultancy, Honoraria. Mailankody:Physician Education Resource: Honoraria; PleXus Communications: Honoraria; Takeda Oncology: Research Funding; Janssen Oncology: Research Funding; Allogene Therapeutics: Research Funding; Juno Therapeutics, a Bristol-Myers Squibb Company: Research Funding. Landgren:Adaptive: Consultancy, Honoraria; Takeda: Other: Independent Data Monitoring Committees for clinical trials, Research Funding; Binding Site: Consultancy, Honoraria; Karyopharma: Research Funding; Janssen: Consultancy, Honoraria, Other: Independent Data Monitoring Committees for clinical trials, Research Funding; Seattle Genetics: Research Funding; BMS: Consultancy, Honoraria; Cellectis: Consultancy, Honoraria; Glenmark: Consultancy, Honoraria, Research Funding; Juno: Consultancy, Honoraria; Seattle Genetics: Research Funding; Pfizer: Consultancy, Honoraria; Merck: Other; Karyopharma: Research Funding; Binding Site: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Cellectis: Consultancy, Honoraria; Juno: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Merck: Other; Amgen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Other: Independent Data Monitoring Committees for clinical trials, Research Funding; Takeda: Other: Independent Data Monitoring Committees for clinical trials, Research Funding; Glenmark: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal